|
I have had a fascinating career as a technical writer and internal communicator. One of my most interesting jobs was editing procedures and batch records1 at a pharmaceutical company that used recombinant DNA to make its most advanced products. Later I wrote operating procedures at a company that made genetic analysis equipment and reagents and was hoping to bring its documentation up to the standards required by U.S. Food and Drug Administration regulations. This was the only way they could transition their products from research use only, good for serving academic and industrial laboratories, to diagnostic use with actual patients in clinical settings.
In working under FDA regulations, one of the things you learn is to believe in things you cannot see. The filters protecting the ductwork that condition the atmosphere in a clean room are either high efficiency particulate air (HEPA) or ultra-low particulate (or penetration) air (ULPA, see the specifications at IEEE Engineering 360). One removes 99.97% of particles 0.3 μm (micrometers, or millionths of the meter) in diameter from the airstream; the other removes 99.999% of particles 0.12 μm, or about a third the size of the HEPA filtration. This is dust you cannot see. These filters will catch pollen, water vapor, bacteria and their spores, most kinds of smoke, and sometimes even an odor in the air. Everything but small virus particles, which generally fall below 0.1 μm.2
For those virus particles, and for anything that happens to drift in through the airlock—although clean room suites are kept under positive pressure, so that any dirt inside will move outward, to the unqualified parts of the building—or that rides on the operator’s clothing after meticulous gowning, the regulations require rigorous cleaning. Since most forms of contamination in the pharmaceutical world involve active microorganisms, like those viruses, the specific cleaning agent is sodium hypochlorite (NaOCl), familiar to every householder as chlorine bleach. It not only removes stains, but its chemical action specifically destroys the long-chain polymers of DNA and RNA, effectively killing bacteria and neutralizing viruses.3 Sodium hypochlorite is highly alkaline—the chemical opposite of acidic—and so it also chemically attacks most surfaces like plastics and metals.4
Alternatively, surfaces and instruments might be washed with 70% ethyl alcohol, which kills bacteria by evaporating so quickly that it dries out the cell membrane before the microorganism can sporulate to protect itself. But not too quickly, though. Some people thought that if 70% alcohol was effective, 90% would be even better. But the more concentrated alcohol evaporates even before it can do its job, leaving the bacteria unaffected. Yeah, and perhaps even mildly drunk.
When working with these disinfectants, the clean room operator uses a wiping material—something like a paper towel, but denser and less prone to linting—under a procedure called “work and turn.” The operator saturates the towel, folds it a certain way, and makes one stroke across the surface to be cleaned. He or she then refolds the towel to expose a new, untouched side, and makes another stroke. The process continues until no unexposed parts of the towel remain, and then the operator discards it and starts with another. The motions for cleaning the surface are prescribed, too. The operator doesn’t just rub the saturated towel around in a circle, like a bartender wiping down the bar. Instead, he or she makes defined, overlapping strokes and never backtracks to cover an already cleaned part of the surface with a section of towel that has already been used. Cleaning a work surface requires diligence and concentration.
If you think this attention to detail is a trifle excessive, neurotic, or obsessive-compulsive, know that the pharmaceuticals this site was making were parenterals—that is, drugs that would eventually be injected into patient’s veins or muscles. Everyone on site repeated the mantra, almost daily, “We make drugs that go into people’s arms, so we have to be clean.”
In the FDA-regulated world, the word “contamination” doesn’t just apply to particles, bacteria, and viruses—dirt you cannot see—but also to the condition of the product’s being exposed, even potentially exposed, to dirt or some other kind of danger. So a batch of product, or an intermediate step in its production, that has inadequate documentation or has acquired some other defect at some point in the operation is labeled “contaminated.” If you don’t know and can’t prove whether the product is pure or not, then it’s not, and it must be discarded or “dispositioned.”5
What conclusions do I draw from all this experience with the finicky, precise, and sometimes whacky obsession with contamination in the pharmaceutical world?
First, our drugs are well made. This care in manufacturing—along with review and oversight of the initial development process, and double-blind testing for safety and efficacy before releasing a new drug to the public—means there’s not a medication made in this country that I would not willingly take on my doctor’s advice. Similar enforcement regimes are practiced in the rest of the developed world. I don’t know that I can say the same for medications made in less cautious countries.
Second, and despite the theme and message hammered home to audiences through now three generations of science fiction and horror movies, products made with recombinant DNA and other advanced biological techniques are not going to get out into the environment, mutate beyond all imagining, and take over the world.
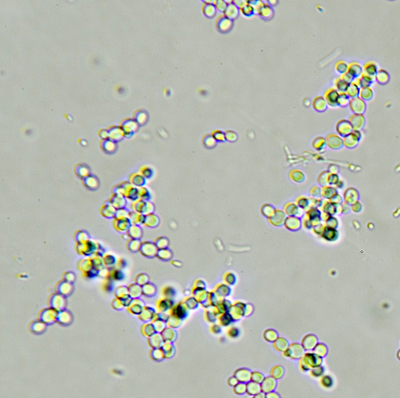
Recombinant DNA is simply the technique of taking a gene that exists in nature, perhaps even in the human genome; isolating it from its chromosome and the embedded system of promoter regions that allow it to function inside the cell’s nucleus; looping it into a plasmid, or circle of double-stranded DNA; and inserting it into the cell body—not the nucleus—of a compatible host cell. There, the host cell’s mechanisms for transcribing DNA into RNA and then translating RNA into proteins proceeds to work on the foreign plasmid just as if it was just a part of the cell’s normal genome. Host cells can be yeasts, bacteria like E. coli, or certain mammalian cells that have long lives and can replicate freely.
The recombinant cells are put into a closed vessel called a “fermenter” or bioreactor, fed a growth medium plus oxygen and other supplements, and allowed to grow. If the protein produced from the plasmid is supposed to be secreted from the cell—such as the human clotting factor produced at our site—then it enters the liquid in the reactor and can be periodically siphoned off and purified as a biological agent. If the protein is normally held within the cell, then the reaction campaign is stopped after a specified period, the cells are extracted and split open, or “lysed,” and the protein is purified from the organic debris.
Fermenter campaigns are a delicate thing. Get the mixture wrong in the growth medium, add too much oxygen, fail to draw off enough of the resulting carbon dioxide, let the temperature vary by a couple of degrees—any number of maladjustments can cause the cells in the bioreactor to die. Oh, and allowing an outside bacteria or other cell type to invade the mixture will contaminate the process, too. Other cells are not only a danger to the identity, safety, quality, and purity of the final product, but they also compete with the host cells for the fermenter’s calibrated resources. Since the host cells are carrying that extra DNA and the burden of making all those copies of a foreign protein, they don’t compete very well.
If recombinant DNA host cells need to be pampered that much inside a bioreactor, which is the safest of all possible environments for them, imagine how vulnerable they must be out in the real world. A bit of used media that carries a few live host cells would pose no real threat if it ever got dumped down a drain—although no pharmaceutical company would be so careless. In an environment crawling with every kind of bacteria, fungi, and other microorganisms, a cruelly burdened strain of E. coli or a baby mouse kidney cell would stand no chance of survival, let alone of attaining wild and uncontrolled growth.
And my third conclusion is that the environment outside the laboratory is a really rough place. I was working at the genetic analysis company after the bioterrorism scare with weaponized anthrax bacilli in the Senate building, and we were tasked with developing a genetic method for detecting the spores in the U.S. Postal Service’s bulk mail centers. As part of that program, we convened a meeting with a number of influential microbiologists to explore what other biological vectors might be weaponized by terrorists and so would need screening.
Most of these experts had just come off a congressional hearing about the recent outbreaks of bird flu, and when we put this question to them, they just laughed. “Mother Nature is the greatest terrorist of them all,” one of the experts said. What he meant was, for every human attempt to culture, refine, and package an infectious agent, the environment itself is inventing a thousand different ways to kill us, like avian influenza viruses, bacteria, molds, and fungi spores. Evolution is at work all the time and, in the aggregate, is a lot more powerful than any human ingenuity. What can get into the lab and ruin your experiment or your production run is far more dangerous than anything that can get out of the lab and into the water supply.
Contamination is everywhere. Your immune system and that of every other human being on the planet is working hard just to keep up. And eternal vigilance is the price of safe drugs and a healthy food supply.
1. In the pharmaceutical business, a “batch record” is the procedure for making, storing, and packaging a product at every step. Unlike, say, a “standard operating procedure,” which simply tells you how to operate a piece of equipment or perform a task in abstract, the batch record includes checks and signoffs at each step in the manufacturing process. It provides written proof that the steps were performed correctly and in the proper order; that the results of every measurement were noted; that critical steps and measurements were also observed and confirmed by a second operator; and that the entire document was reviewed by the department supervisor at the time of production and by a representative from quality assurance before product release.
Batch records apply not just to the product itself but also to any part of the plant and its operation that might affect the product’s identity, safety, quality, and purity. So the operators will complete a batch record for cleaning tanks, sterilizing hoses and utensils, calibrating equipment, and even mopping the floor in the production suite.
2. Of course, if a virus gets airborne at all, it will probably be riding on a water droplet from a sneeze or a dust particle derived from a flake of skin.
3. Because a virus is not technically alive, outside a host cell, you can’t “kill” it. But you can stop it from doing whatever it’s going to do, which is the same thing.
4. But that’s not the worst hazard in the manufacturing suite. At the pharmaceutical company, we used to clean mixing tanks with heated sprays that alternated hydrochloric acid (HCl) with sodium hydroxide (NaOH)—an acid followed by a base. This would scour out any protein residue left over from the manufacturing process. And then the procedure followed it all with pressurized steam at 122°C. You might worry about putting these acidic and caustic flushes down the sewer drain, but first they were sent to a holding tank, where the two chemicals neutralized each other, producing salt water.
5. And don’t believe that means just thrown away. A dispositioned batch has a documentation process all its own, so there is no possibility that it might get back into the product stream.